What all educators need to know
By Lauren Zucker, PH.D.
As an educator and a new mother, I struggled to envision what pumping breast milk might look like when I returned to work. I thought of friends who told me they pumped while driving to school, or while scarfing down their lunch in a supply closet. I worried that my rotating teaching schedule, further complicated by the COVID-19 pandemic, couldn’t accommodate the regular breaks I’d need. A private person in some ways, I struggled to imagine how to approach this conversation with my colleagues, my administrators and my students.
For those who have never pumped milk themselves, or witnessed it, it can sound fairly straightforward and mechanical. Attach a machine to the body, turn on the pump, extract the milk. In my lived experience, however, it is a lot more complicated.
At the new parent support groups I attended, working mothers described the challenge of finding the time and space to pump in the middle of a hectic workday. For those who were lucky enough to secure a comfortable pumping location and block off the time they needed, many found themselves yielding less milk during those pumping sessions than what their babies needed in their absence.
The end of my parental leave on the horizon, I reached out to local experts to help me prepare for pumping at work. In these conversations, I learned that many educators may not be aware of their rights to pump at work, and many choose not to do so because of the associated challenges. The article that follows is a product of my efforts to navigate this process as an NJEA member and new mother in the time of COVID-19.
I conducted one-on-one interviews with four New Jersey experts in maternal health to cover the medical, and legal and interpersonal aspects of pumping or expressing milk. I spoke with Jill Wodnick, a maternal health educator and advocate, Ellen Maughan, a retired attorney and Co-President of New Jersey Breastfeeding Coalition, Carmen Baker-Clark, an Internationally Board Certified Lactation Consultant (IBCLC) and manager of the lactation program at the CarePoint Health Hoboken hospital, and Allyson Murphy, an IBCLC whose work with educator clients led her to develop recommendations for school-based lactation policies. Our discussions covered topics such as lactation space considerations, strategies for overcoming common obstacles, and tips for communicating with administrators. In some cases, their responses have been abridged and/or edited for clarity.
The Basics of Pumping at Work
Who is entitled by law to pump milk at work?
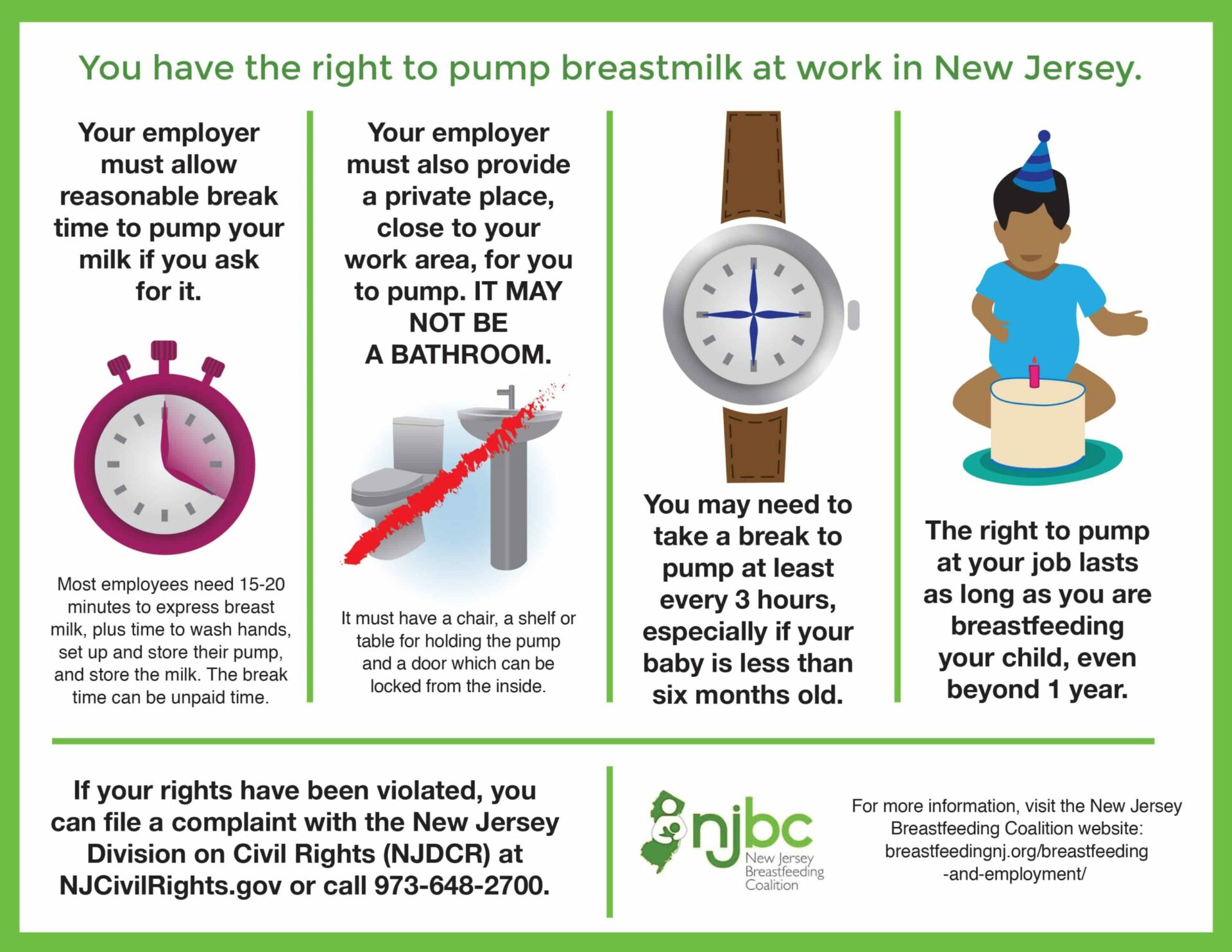
Ellen: Every breastfeeding employee is covered by New Jersey’s legal breastfeeding protections, which are stronger than existing federal law. Breastfeeding employees have workplace pumping protections under the New Jersey Law Against Discrimination (LAD), which was amended in 2018 to include breastfeeding. The LAD covers all New Jersey hourly or salaried employees, with the possible exception of federal employees, who may be covered only by provisions of the Affordable Care Act (ACA).
Where can employees pump milk?
Ellen: The law requires that the employer provide a reasonable break time and a private place to pump that’s not a bathroom and is in close proximity to the employee’s workplace. In the federal law, a private place is considered to be a place that’s shielded from view with a door that can be locked from the inside.
The New Jersey breastfeeding law, N.J.S.A. 26:4C-7 further defines lactation room as “a sanitary room, other than a restroom, which can be used by a mother to breastfeed her baby or express milk in private, and which includes an electrical outlet, a chair, and nearby access to running water.”
Carmen: It should not be in the nurse’s office, because that pumping mom would be exposed to every possible germ that’s in there, and then she’d be bringing it back to the baby.
If a mom is working virtually from home and breastfeeding her baby directly is an option, she should absolutely do that over pumping because the baby will do a better job of emptying the breast, it will take less time, and be less complicated.
Allyson: A pumping room would ideally also have a refrigerator that’s used only for storing milk. You need to have outlets because pumps need to be plugged in. You need a chair that you can sit comfortably in for 20 minutes, you need a table to be able to put the pump and the bottles on. Soap and paper towels at the sink, and, ideally hot water to be able to wash your hands and your pump parts.
Some people want to be really private, and they don’t want anybody else in there with them. So there should be a schedule so that those who are breastfeeding know who’s using the room and when. Other people are comfortable with sharing with a coworker, but then you want to think about how you divide that space. Do you have partitions? Do you have two tables that face opposite ways?
Even with a locking door, look for some way to create a visual barrier, such as a folding screen. So if the door gets accidentally opened, you don’t have a hallway of students looking in and seeing Miss Smith hooked up to a pump. Everyone’s biggest anxiety is having the students walk in on them. I’ve had some clients whose supervisor or principal let them use their office, probably because they themselves or their partner had nursed in the past.
How often should working mothers pump milk?
Ellen: The law says “reasonable” pumping breaks and that of course depends on the mother’s own situation. What is reasonable depends on the age and needs of the baby and how often the mother is pumping. In general, the number of pumping breaks needs to approximate how many times the mother would feed the baby if the baby was with her. Most full-time employees need to pump three times during a work day: a morning pumping, a mid-day pumping, and an afternoon pumping. If the baby is exclusively breastfed and below the age of six months, for example, most mothers need to pump at least every three hours.
Carmen: A mom also needs to also take into account her commute time so that will extend the separation from her baby.
Allyson: Educators’ changing schedules can make pumping difficult. Special schedules, such as half days, assemblies, and emergency drills, also create challenges. Lactation works on supply and demand, and you have to have certain intervals to your pumping. When I have clients whose schools are on rotating schedules—when, for example, sometimes your pump time is at 8 a.m., and sometimes your pump time’s at 9:30 a.m.—it’s really hard for your body to adjust. Our bodies need a lot more predictability in those time frames.
What is an appropriate amount of time to go between pumping sessions, and what are the risks of going too long between sessions?
Carmen: Going too long between pumping situations can be very painful and uncomfortable. There should be no more than three hours between daytime pumping or between feeding sessions. If you go much longer than that, the body might get into a feeling of over-fullness, that could lead to clogged ducts, and if that clogged duct remains untended to, that can cause mastitis or a breast infection. If the milk isn’t really frequently removed, that mom may experience a decrease in milk supply. If a mother is teaching a class, and she has not been able to pump her breast, and the breast becomes quite full and engorged, it becomes very firm and painful and can begin to leak and soak through her clothes.
What safety and hygiene protocols should be considered for lactation rooms and pumping during the COVID-19 pandemic?
Ellen: In their guidance document on “Care for Breastfeeding Women” (bit.ly/carebwcdc) in the context of COVID-19, the CDC refers to these general recommendations for cleaning and disinfecting facilities (bit.ly/cdcbuilding) in many settings, including lactation rooms.
Carmen: The space should be cleaned in between uses—particularly the surfaces and the places where parents are setting themselves up for pumping. Wiping down surfaces, thorough hand-washing, and thorough washing of pump parts is another challenge. A lot of moms feel like washing all these parts takes time takes away time from their pumping time. So there’s a common practice of pumping and then not the washing parts—just putting them into a Ziploc bag and storing them in the refrigerator, reusing them again at the second and third pumping session, before washing them one time at home after work. But in the current environment, that would be tricky. We should be washing in between each pumping session because we don’t know what our exposure to viruses might be in this space.
Pumping moms must practice careful hand-washing, more than ever, and take the time to wash their hands for 20 seconds with soapy water. Hand sanitizers don’t cut it. And you need hot, soapy water to clean the pump parts, but if there’s only warm water, that can work. It’s also best to have a window that you can open to let fresh air in with blinds for privacy.
How does milk supply (someone’s capacity to produce breast milk) work? And how can stress affect milk production?
Carmen: Breasts make milk based on a response to the baby’s needs. So if the baby is feeding 10 to 12 times in a 24-hour period, milk is going to be removed at least every two hours, and the milk will refill as soon as it is removed. If the baby’s only feeding five times in a 24-hour period, then the breast is only going to make milk for those five times. If mom pumps milk three times during her work day, then she will make milk for those three times on a regular basis. If the baby needs more milk than what was removed those three times, then she doesn’t have enough milk for her baby.
If a pump or a baby takes out all the milk that’s in the breast, then every single mammary gland in the breast will refill itself. But if only half the mammary glands are emptied and half are left full, then only the ones that are empty will refill, and the ones that remain full will get the message that “you don’t need to make milk here because nobody’s emptying this.” So that’s how supply decreases.
Also, stress can be a factor. If a mom is very stressed, it affects her release of oxytocin. That’s the hormone that causes mammary glands to contract and expel the milk forward. A mother who is experiencing stress while trying to pump at work might make less milk because she’s not relaxing and allowing the body’s hormones to work.
Though the law requires separate break time for pumping, some educators choose to multitask—for example, by grading papers or eating lunch while they pump. What do you think of that practice?
Carmen: Different women feel differently. Some women will pump anywhere comfortably, and some women really need to be in a private, secluded place where she feels like no one’s going to invade her privacy. Some teachers, for example, could take care of some grading or some projects on the computer while pumping discreetly. Even though it’s supposed to be a break time, she could multitask with one of the more portable pump sets, like the Baby Buddha, or the Zomee, Ameda Mya, or the Minuet. They’re very compact, but also very powerful and can connect to your computer through a USB cord.
But many moms cannot multitask while they pump. First of all, a pump is impersonal. You can train your body to let down (release milk) to a pump, but it’s always easier when you take the time to think about your baby. Sometimes you need to actually concentrate and think about your baby, look at pictures, or look at videos of your baby to help you have that oxytocin letdown. Second of all, a mother might actually need to use her hands on her breasts while pumping to help speed up the ejection of milk. If she doesn’t have a private space, or she feels like her privacy will be invaded suddenly, then she might not be able to let down as much milk as she needs to fully empty her breast. She could spend 20 minutes on a pump and not get much milk at all.
Privacy is very important for some people, and less important for others. But it’s not about how they can function. It’s about what they deserve. They all deserve the same amount of privacy and considerations.
Ellen: For some mothers, multitasking while pumping is not physically possible and can negatively affect their milk output. I recall talking to friends who are lawyers who were pumping and doing their legal work at the same time. With the stress of going back to work and those additional needs, for some mothers, their milk supply really starts to tank, despite their best efforts. Working as a lactation consultant, I could try so many different hacks and tips for mothers, and sometimes that additional hand is really needed. Some mothers have hands-free pumps, but generally they’re not the type of pump covered by insurance that most mothers are getting.
Allyson: I think that prep periods are for prep. That’s your job. That’s not your break. I know it’s hard to find coverage for teachers, but you should have a break for 20 minutes to pump and not be trying to eat your lunch and plan your lessons and do grading while you’re also pumping. I think teachers’ days are so tightly packed that to be asked to use your prep periods as your only pumping time doesn’t respect that prep periods are necessary for teachers to get their work done. And prep periods are not always at the same time. This is another huge challenge.
Another one that comes up with teachers a lot is duties. I’ve had lots of clients say, I’m going to ask my principal if I can get out of doing lunch duty so that I have that time to pump and the administrator says no. I also understand it from an administrative standpoint because you need to cover these things, but I think we need to give more flexibility to and give priority to people who have just come back from having a baby. We put so much pressure on people to breastfeed in this country. And we don’t do a very good job supporting them.
Why is a woman’s right to pump at work important?
Ellen: Breastfeeding is a social justice issue for many families. Without the right to pump at work, mothers who would want to but cannot afford to stay home longer with their baby, are prevented from feeding their babies as all world health authorities recommend.
Jill: The indicator of a healthy community is maternal infant health. It gives a snapshot of the tempo of how we are doing as a community, as a culture, as a society. This includes both the social-emotional journey as well as physical assessments. The health and well-being of the infant-parent dyad in pregnancy, giving birth, and in the immediate postnatal period tells a story of where resources are being allocated. In New Jersey, we need to move our state from worst to first in terms of improving maternal infant outcomes. So we can absolutely honor individual health privacy as well as scale up visible resources so all expectant and new families-and that includes partners, fathers, and grandparents will-have less obstacles in resource navigation.
There are incredible outcomes when an infant gets exclusive breast milk. When women are supported to breastfeed, they reduce their risk of breast and ovarian cancer; they reduce their infant’s risk of asthma and obesity.
Carmen: It’s a way for her to stay connected to her baby and make her feel like she’s doing something for her baby even when she’s at work.
It’s a very difficult thing to go back to work under any circumstances and leave a baby. There’s a separation that the mother’s going to mourn. And so there’s a lot of stress involving not just the planning of how am I going to continue to pump for my baby, but just the idea that she’s going to be missing her baby, missing developmental milestones, missing fun moments and conversations, like when they start babbling or crawling or climbing or walking. Though we have technology to help capture these moments, it’s not the same as being there to mother your baby. Maintaining breastfeeding and milk production is a way of staying connected to her baby. Knowing that your baby is receiving your milk might make that mom feel a little bit better about leaving that baby to be taken care of by somebody else.
Aside from their legal obligations, why should employers support employees who are pumping?
Jill: Supporting the needs of pumping employees is really a short time in the trajectory of someone’s career, but the support, the encouragement, the assistance that happens during pregnancy and lactation is really going to change the trajectory of the rest of that career. The needs of a pumping employee truly may be four weeks, or four months, but it’s not going to be forever, and it’s going to change health outcomes. So we have to understand that this cooperation and the continuity of care is really essential because it’s going to impact the health and well-being of that employee and their child.
Allyson: This is a slice of time. If I graduate and teach from then until I retire, I’m likely going to teach for 40 years. Many educational support professionals devote their whole working lives to schools.The average person in New Jersey has two babies. You’re talking about two years out of a more than 40-year career where I need some accommodations. If we can think about this as community spirit, that we’re going to help each other out during this slice of time when you need a little bit more freedom and flexibility. We should also give our administrators support so that they can that they can allow that flexibility for school employees.
Preparing to Pump at Work: Advice for Breastfeeding Mothers
How does a working mother figure out how much milk to leave for her baby? Should she begin pumping before her return to work?
Carmen: We determine how much milk to leave based on the baby’s age and weight. If you have a 10 lb. baby, the mom is going to need to feed that baby 20-25 ounces in a 24-hour period. So if she’s going to be gone for nine hours, that baby will need 3-4 bottles during that time period. To figure out a range of what your baby might need, take the baby’s weight and multiply it by two. That’s the lower limit of the range. Then add half of the baby’s weight to that number, and that’s the upper limit. So if you have a 10 lb. baby, multiply the baby’s weight by two (10 x 2), and you get 20 ounces, which is the lower end of the range. Add half of 10 lbs. (five) to that number (20 + 5) and you get 25 ounces, which is the upper end. On average, a 10 lb. baby will consume between 20 to 25 ounces of milk per day.
Ideally, she should begin pumping a month in advance of her return to work. She should always pick the same time of day to pump (e.g., mid-morning), and store that milk by labeling it with the time and date, and freezing it. If she does that for 30 days prior to her return, she should have the first few days’ worth of milk that she needs to leave behind for her baby and a backup stash to give her the confidence that she has enough milk, if, for whatever reason, she isn’t able to pump as much at work. At minimum, she should have at least a few days’ worth of pumped milk—at least 20 to 30 ounces in her freezer.
How can a mother who is planning for a return to work anticipate her pumping schedule?
Carmen: To anticipate the times she might pump, she can use her baby’s feeding records as a reference, but you have to remain flexible. I think many of the moms who succeed are able to block out a specific amount of time during the workday to do the pumping. Let’s say a mom has a baby that, when she’s home with them, would nurse every two-and-a-half to three hours in a rather unpredictable way. At work, she’s not going to be pumping at the same time that her baby may be feeding. She’s going to have to find a happy medium and just put herself on a schedule. Her body will adjust. So ideally, she can space it in a way that’s regular and predictable for her. If she’s doing a five-day work week, and she always pumps at 10:30 a.m., 1 p.m., and 3:30 p.m., then her body will regulate to that schedule and she’ll be able to get enough milk at that time.
Many working mothers experience a drop in milk supply when they return to work. What can they do to boost their supply?
Carmen: When you’re home, go back to just breastfeeding the baby on demand. Follow your baby’s feeding cues as opposed to feeding on a schedule, because the baby will most likely feed a lot more frequently, which will bring the milk supply back up to where it needs to be for the baby. Also, prioritize skin-to-skin contact as a way of reconnecting. Babies benefit from that contact and moms do, too. Build it into the routine—for example, get in the tub with your baby. There’s a million things that women have to do, and it’s amazing what women who are going back to work are expected to do while taking care of children at the same time. But try to prioritize spending some time with the baby and maximizing that time in the morning, evening, and overnight.
How can mothers most effectively communicate their pumping needs to their employer?
Ellen: Ideally, I would hope when a pregnant educator approaches the school district about taking leave for childbirth, the school’s written lactation policy would be made available to them through human resource channels. If not, the mother should see if there’s a process for requesting lactation accommodations in place with her employer—whether you go to HR, for example, or you go to your supervisor.
Whenever a mother is approaching their employer, it’s always best to have a very positive “can do” sort of attitude. Wherever possible, supply some examples of how other similar businesses or employers have handled the situation. And she should explain, as calmly and positively as possible, what her needs are. The Office of Women’s Health has great resources on their website, including “The Business Case for Breastfeeding,” (bit.ly/owhbusiness) and information showing how specific industries (bit.ly/owheducation) addressed workplace pumping needs. The educator can say to the employer, “This is the way other school districts are doing it. Here’s how they tackled these challenges.”
Carmen: I would bring in the law that supports her pumping in the workplace (see bit.ly/nj242-26). And maybe some information on the benefits of keeping her baby breastfed. Besides being able to continue to provide the best source of nourishment for her infant, she is also keeping her baby well, so that she doesn’t have to miss work to take care of a sick infant. That’s one big huge benefit to mention to supervisors that might encourage them to set her up in a comfortable place to pump.
Allyson: It can be awkward if you’re a shy person. It can feel like a very personal thing. You’re talking about your body, and you’re talking about your breasts. One thing that I say to clients all the time, is that you really do need to advocate for yourself. You have to not be afraid to stand up for yourself and to ruffle some feathers. I think that’s a lot easier said than done even if you’re a tenured teacher or have due-process rights as an ESP. If you’re the newest person in the door and you don’t yet have tenure or due-process rights, it can be nerve wracking to demand that you need this time. Also, reach out to colleagues who had a baby in the past five years and talk to them about whether they pumped, and if so, where they pumped.
What resources do you recommend for mothers who are pumping at work?
Carmen: I recommend staying connected with their lactation consultant and texting them about whatever challenges that may be happening. If she needs to find one in New Jersey, she can look at ZipMilk.org, ILCA.org, and IBLCE.org. A lactation consultant can support a working mother in many different ways. During a visit, we cover topics such as how often she is pumping, how much milk the baby needs, what kind of pump she is using and if it fits properly, how to maximize milk production, how to strategize nighttime parenting to help everyone get more sleep, etc. A lactation consultant can help a breastfeeding mother figure out how much milk her baby is drinking by taking a pre- and post-feeding weight with a very precise scale right before feeding, between sides, and after feeding the baby to calculate how much milk is transferred on each side and over the full feed. During that weighted feed, there’s an opportunity to review positioning, practice getting a deep latch, and help the baby drink more effectively to empty the breast and maximize production.
There’s many places to find information online, but I always recommend any resources that are research-based. For example, Kellymom.com, is a long-standing website that’s always offering evidence-based information. There are Facebook groups that offer moms platforms to just talk and be heard by fellow moms who are supportive and caring. But they can be tricky because some of the advice might have benefited the mother offering the support but may not be the right advice for the mother receiving the advice. I always give a word of caution to seek the help of a professional.
There are wonderful support groups for mothers. It’s also another great way to staying connected, particularly if a mom gets the opportunity to work virtually, or she’s able to take a few minutes of her workday to connect to a support group during her break time and ask questions to the facilitators, or to talk to other moms who might be in similar situations as she is and brainstorm about how to make things better.
Ellen: Educators can find legal resources about their breastfeeding and lactation rights on the New Jersey Breastfeeding Coalition (NJBC) website at breastfeedingnj.org. La Leche League (llli.org and lllusa.org) is a great organization for breastfeeding mothers that offers peer-to-peer support through phone-based support and group meetings in both the daytime and evenings.
Allyson: There’s also a great book called Work. Pump. Repeat., by Jessica Shortall.
Improving the Pumping Experience for New Jersey Educators
Recent updates have made the New Jersey breastfeeding laws even stronger. What could we do better?
Ellen: Make the pumping break time paid for all employees. Neither the federal law or state law requires pumping break time to be paid, though some employers will allow it to be paid. But others, especially for hourly employees, require that they punch out. It can be difficult for many families to afford unpaid break time. If a mother can come in early and make up some of the time and stay late then it can work, but it will lengthen her day and the amount of time that mother is away from her baby, which creates additional challenges.
Allyson: I have a lot of clients who are teachers who end up weaning (stopping breastfeeding) earlier than they would really want to, well before that 12 months that they would want to try to continue if it worked for them. But they just don’t even attempt to continue nursing because it just feels completely undoable to pump as an educator. I have seen that so many times.
In 2018, I wrote a report (see bit.ly/njschoolpumping) with recommendations to help school districts develop policies to support breastfeeding employees. No one should have to reinvent the wheel every time they come back from maternity leave. You have enough stress about leaving your baby, coming back to school, and being an educator, which is stressful enough as it is. If you’re going back now, in the wake of COVID, you should not have to invent your own pumping schedule and plan. It should already be in place in your district. When you tell your supervisor that you’re expecting a baby, they should alert HR, and before you come back, they should contact you and help you figure out how to pump.
I think if we had a year of paid maternity leave, this wouldn’t be an issue. But we have people go back to work 12 weeks after their babies are born. We recommend nursing for 12 months. The math just doesn’t add up. When they do go back, we don’t always support them in nursing for those other nine months of that first year.
Jill: Even though education is historically a female-dominated profession, there’s a missing gap for New Jersey public educators about making maternal-infant health needs more visible. In New Jersey, we need an immediate reimagining of the delivery of maternal health, and that includes eliminating obstacles to information about breastfeeding laws, including the rights of breastfeeding and pumping for public school employees. First, we need to get a baseline assessment of what the experience is at a building, district, and county level for New Jersey public educators to learn the barriers and opportunities for seamless coordination to be compliant with the law.
It doesn’t have to be an either/or. We can keep strong teachers and ESP building relationships with their students and engendering transformation and wonder in the classroom and throughout the school, and we can acknowledge the critical and unique needs of maternity care and breastfeeding support in New Jersey.
What do I tell my students?
A staff person should never share personal health information with students. From an employment perspective, to do so could set an employee up quite easily for some form of discipline. However, in consultation with your local association representative (AR), carefully review board of education policy to see if it addresses whether breast pumping school district employees may explain to students the reason for their breaks. If such policies exist, work with your AR and your administrator to discuss what you tell your students. Be sure to have any agreement in writing and make sure your local association leadership is included in the agreement.
What if my rights have been violated?
In 2018, “breastfeeding” was added as a protected class to the Law Against Discrimination (N.J.S.A. 10:5-12) (LAD), which means it is illegal to discriminate against an employee on the basis of their breastfeeding status.
If you are experiencing problems with breastfeeding accommodations at work, you should talk to your union representative with your supervisor to try to work it out. The process is an interactive one and the more questions you ask if the initial request is denied, the more likely you will be accommodated. Your regional NJEA UniServ representative can also support your requests.
But if the employer refuses and continues to deny your right to a private space to pump, an employee may file a complaint with the New Jersey Division on Civil Rights (DCR) or in the Law Division of the Superior Court of New Jersey. If someone suspects their workplace breastfeeding rights have been violated, they can contact the New Jersey Division on Civil Rights (NJDCR) at nj.gov/oag/dcr/localcontact.html or the U.S. Department of Labor at dol.gov/agencies/whd/contact, or seek legal counsel. Also see nj.gov/oag/dcr/filing.html and DCR’s Frequently Asked Questions at nj.gov/oag/dcr/faq.html for more information.
If the DCR or Superior Court finds the employer to be in violation of the law, remedies may include an order restraining the discriminatory action, back pay, damages for pain and humiliation, and attorney’s fees. Punitive damages are available in Superior Court actions. Bear in mind, however, that legal challenges take time.
Law requires annual DOE implementation report
Recent updates to New Jersey law (N.J.S.A. 26:4C-3) require the Department of Education to submit by Aug. 15, 2020, and annually thereafter, a report to the governor and Legislature about “lactation-related policies that have been implemented at schools, universities, and colleges,” including “the manner in which those policies were communicated to students, parents, and guardians.” The first report, required to be posted on the DOE website, has not yet been released.
Lauren Zucker, Ph.D., teaches English at Northern Highlands Regional High School in Allendale. She teaches education courses at Fordham University and Drew University, and has served as membership chair for her local association. Her op-ed on the importance of telehealth support for breastfeeding mothers recently appeared in NJSpotlight (see bit.ly/njspotlightzucker). At laurenzucker.org, she writes about teaching and research. She can be reached at lauren6@gmail.com.
Ellen Maughan, JD, IBCLC, is a retired attorney who has been supporting breastfeeding families in health care settings and the community for 25 years. Ellen currently serves as co-president of the New Jersey Breastfeeding Coalition (breastfeedingnj.org) and is an adjunct professor at Drexel University. Most recently, Ellen managed the New Jersey Breastfeeding Strategic Plan project in partnership with the NJ Department of Health.
Jill Wodnick is a childbirth educator and policy expert who works at Montclair State University on improving maternity care. She has advocated for respectful, equitable maternity care for nearly twenty years. Her previous experience as the director of community doula programs helps her center the voices of women and families from diverse backgrounds in local, state and federal policy proposals. Contact her at JillWodnick.com.
Carmen Baker is an International Board Certified Lactation Consultant (IBCLC 2005) who offers loving lactation support to new and expecting families via her North Jersey practice Breastfeeding Momma (breastfeedingmomma.com). Through her work as manager of the CarePoint Health Hoboken Lactation Program, she supports expecting and newly delivered families, leads staff education, and runs a New Moms Support group.
Allyson Murphy, an International Board Certified Lactation Consultant (IBCLC), offers warm lactation support to expecting parents and new families through her North Jersey practice Lactation Ally (lactationally.com). She helps clients meet their feeding goals and runs a postpartum support group that offers care and community. Allyson recently authored a report (bit.ly/njschoolpumping) to help school districts create written policy to support pumping employees.
